Giant Cell Arteritis: a rheumatological emergency

In rheumatology, there are few super-urgent, “life or death” situations. I like it that way.
Most times when urgency is involved, it’s usually relates to a severe side effect or to a severe infection. Rarely, it relates to the manifestations of difficult disease processes, such as vasculitis (where there is inflammation of blood vessels causing a lack of blood supply to the organs the vessel supplies).
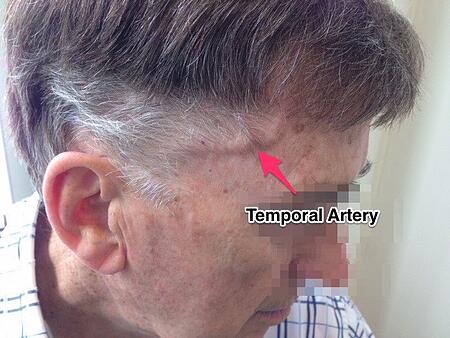
Last week, I took an urgent call from a local GP. She’s a very astute GP and when faced with this older gentleman presenting with headaches, fever, a feeling of being unwell as well as a lot of tenderness at his right scalp, she immediately suspected this relatively rare disease.
Giant Cell Arteritis (read more about GCA here).
This is an emergency situation and should be treated as such.
Giant Cell Arteritis can lead to sudden, permanent loss of vision and prompt treatment can prevent it.
We discussed his case over the phone and these were organised urgently:
- A same-day appointment with an Ophthalmologist to examine the eyes and to arrange biopsy of that very swollen, painful temporal artery -> the diagnosis was confirmed with classic pathological changes on the biopsy.
- Immediate commencement of high dose Prednisone. He was given 75mg daily of Prednisone and his symptoms improved dramatically over the next few days.
- Measurement of inflammatory markers -> the blood tests did show markedly elevated ESR and CRP, blood proteins which increase in this disease due to the vasculitis.
What about my role as a rheumatologist?
Well, the good news with this disease is that the use of corticosteroid, Prednisone, helps immensely. The problem is that the antidote is Prednisone. I’ve already written about the 2-edged sword that Prednisone can be (here's a link to posts re corticosteroid). And this is definitely the case at these higher doses.
So, in this disease, the rheumatology management consists of:
- Managing the gradual reduction/taper of the dose of Prednisone. Steroid reduction can be difficult. Many rheumatologists, including myself, use Methotrexate to help with this steroid taper. Methotrexate acts as a “steroid-sparing” agent.
- Predicting and trying to limit or avoid the side effects of Prednisone, for example:
- Checking the bone density and then trying to prevent steroid-induced osteoporosis/bone loss.
- Anticipating the weight gain and effects on metabolic syndrome and instituting measures to try and help. Attention to diet and nutrition is important as well as exercise.
- Anticipating the weakness of the proximal muscles (thighs, upper arms) and instituting appropriate maintenance and strengthening exercise.
All this needs to be done, while trying not to reduce Prednisone too quickly to avoid a flare in the disease, as a lack of control on the inflammation causes many unwanted symptoms, and in particular, increases that risk of sudden blindness.
Have you any experience of this condition?