Rheumatology? What’s that?

As I was growing up post-medical school, I was going to be a cardiologist. My first few years were spent on wards, dealing regularly with angina, blood pressure problems, and attempts to find blood vessels to harvest the precious red stuff or to stick cannulaes into. I thought it would be cool to be the heart doctor who rushed in at night to save dying heart muscle. I’d perform life-saving angiograms, controlling guide wires and balloons to open up blocked arteries. Cardiologists also seemed to wear expensive suits and drive nice cars.
In my 4th year post-medical school, I was assigned a term with the rheumatology team. My mentors were decent, caring individuals.
I was surprised to find that I enjoyed the wide variety of work and importantly, the long-term relationships rheumatologists have with their patients. It soon dawned on me that rheumatology was very much an outpatient specialty, providing an opportunity to have less to do with a hospital system that was getting progressively more anaemic and definitely more frustrating to work in.
Nice patients; interesting, diverse work; a decent lifestyle choice. I turned.
For the record, most people don’t know what rheumatologists do.
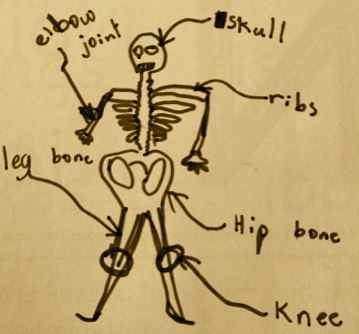
Rheumatologists are arthritis doctors, who deal with both mechanical/degenerative joint diseases and inflammatory joint diseases. In addition, we deal with most problems affecting muscles, tendons and ligaments. We deal with diseases of the spine and diseases of the immune system.
You may know someone with gout, or someone with a work injury, or someone with strange aches and pains to the point they’ve had to see lots of different health practitioners without satisfaction. You may have a dicky knee or been told you have rheumatoid arthritis. We deal with all of these, and more.
Our brief is very large. Our tools are typically a thorough history, a good examination and an investigative mind. We actually communicate.
Rheumatology is entering a golden age. Technological improvements now mean that the best investigative tests are routinely available. Treatment options have become highly advanced. We have also learnt to use our older medications in more efficient and in novel ways. The pace of scientific endeavour has never been faster.
A standout example would be the treatment of ankylosing spondylitis. This is a potentially crippling disease causing widespread spinal pain and stiffness, eventually leading to a very rigid spine. Once a terribly frustrating disease to treat, there are now “biologic” agents which can “switch off” the disease within weeks.
Apart from medication advances, there has been a clear emphasis on multi-disciplinary care and a much more patient-focussed approach to disease management. Our clinic, with its team approach, strives to refine this process of delivering efficient, connected care. Great treatment for rheumatic diseases, and indeed, for many diseases, requires more than any one individual can provide.
Rheumatologists are traditionally conservative, caring and communicative physicians. We still are, but in the 21st century, we are also increasingly effective.
Dr Irwin Lim is a rheumatologist and a director of BJC Health. You should follow him on twitter here. Arthritis requires an integrated approach. We call this, Connected Care. Contact us.